PROVIDERS
Would you like to build your capacity to address perinatal depression and anxiety in your work? We offer a variety of learning options, live and self-paced, to help health care, mental health care and social service providers gain the skills needed to support the emotional well being of new and expectant families.
PARENTS & FAMILIES
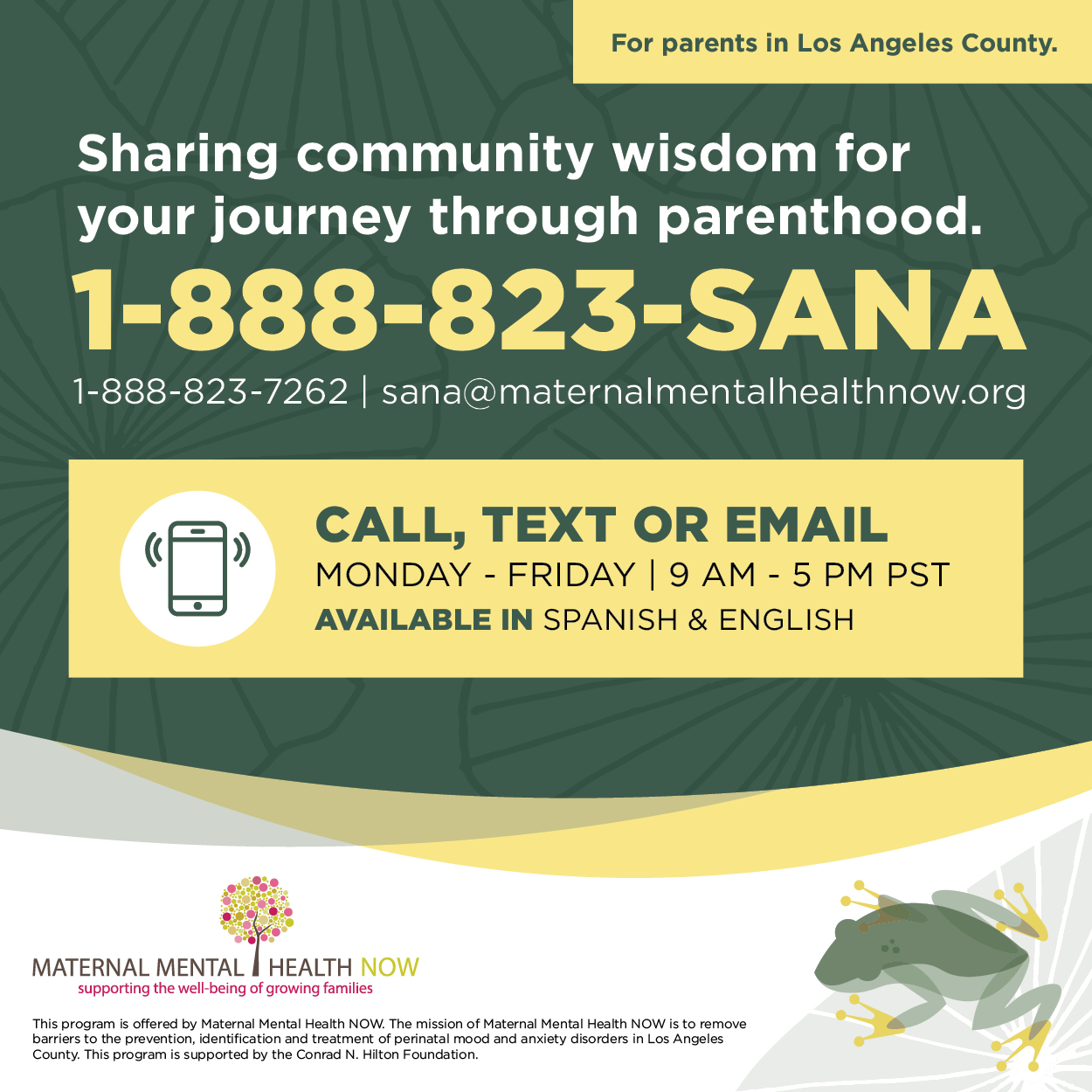
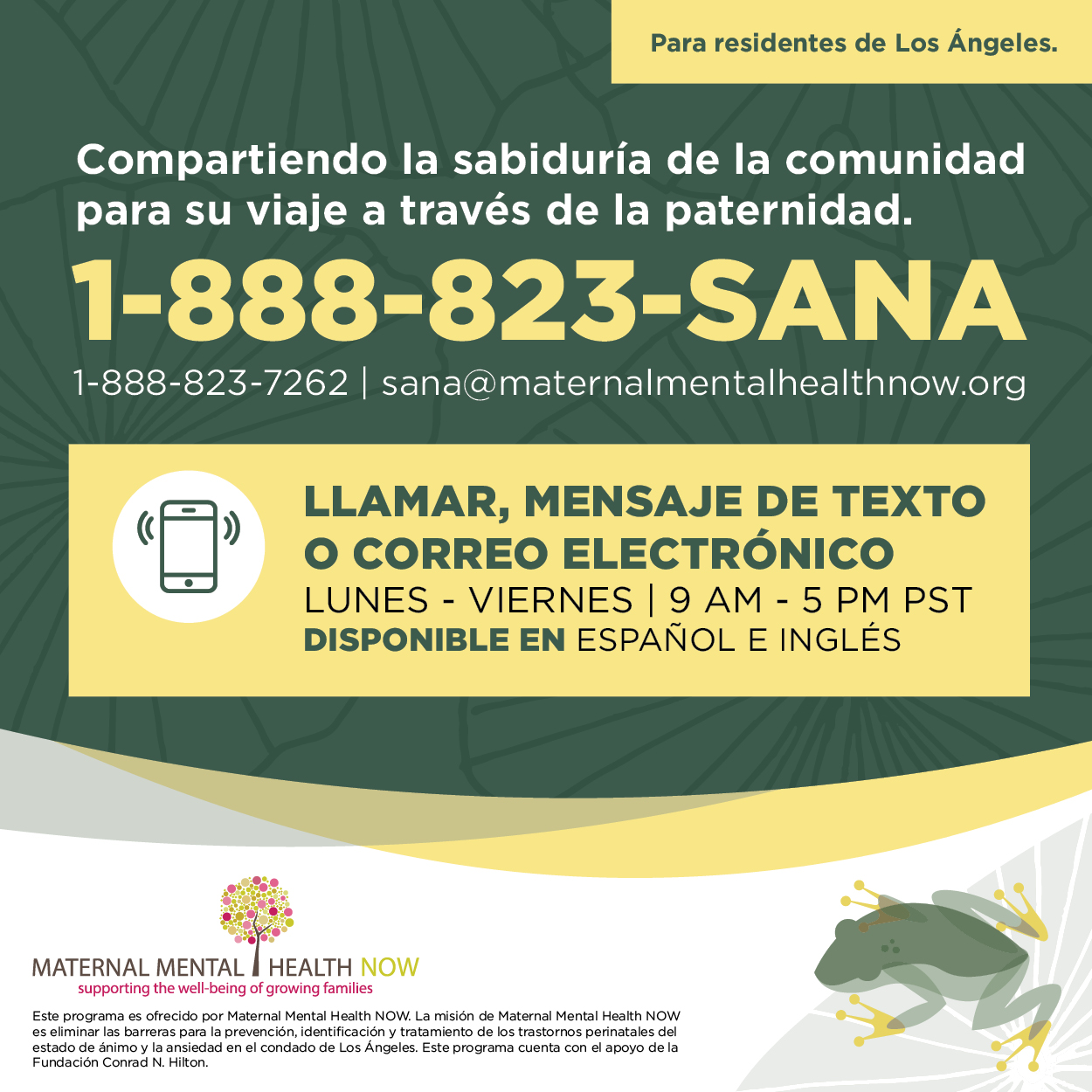
Have you or a loved one recently welcomed, or are about to welcome, a child into your family? Depression and anxiety during pregnancy and postpartum affect all family members. We offer information, a self-care app, and a directory of resources so you can find support for yourself and your loved ones.
PARENTS & FAMILIES
Have you or a loved one recently welcomed, or are about to welcome, a child into your family? Depression and anxiety during pregnancy and postpartum affect all family members. We offer information, a self-care app, and a directory of resources so you can find support for yourself and your loved ones.
Perinatal mood and anxiety disorders consist of depression and anxiety that affect any new mother, father or caregiver anytime between conception and 1 year postpartum.
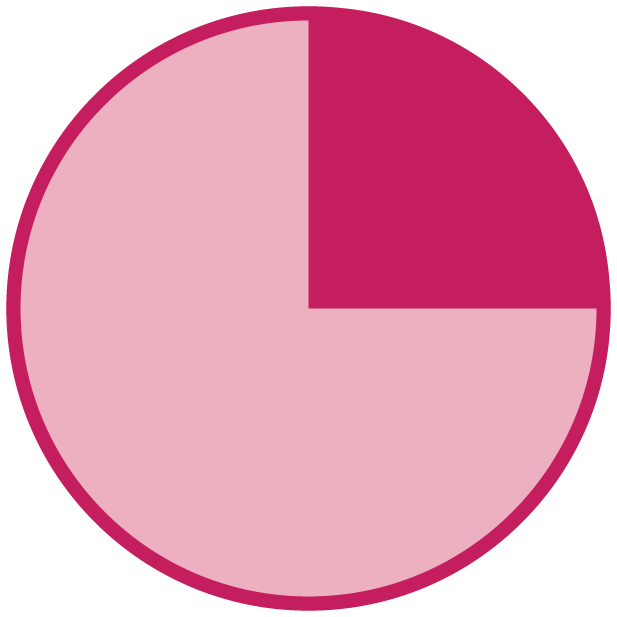
In Los Angeles County, 25% of birthing people reported a depressed mood during pregnancy and/or the postpartum period.
LAMB Survey, 2016

Rates are highest amongst African American and Medi-Cal patients.
LAMB Survey, 2016

Across the state of California 72% of people with perinatal depression or anxiety never received counseling or treatment.
Listening to Mothers Survey, 2018